On This Page:
Key Takeaways
- Between 1969 and 1972, Prof. David Rosenhan, a psychiatrist at Stanford University, sent eight pseudo-patients to 12 psychiatric hospitals without revealing this to the staff. None of the pseudo-patients had any symptoms or history of mental disorders.
- In all 12 instances, pseudo-patients were diagnosed with a mental disorder and hospitalized. In no instance was the misdiagnosis discovered during hospitalization.
- In some of the 12 hospital stays, pseudo-patients observed significant deficits in patient-staff contact.
- In a follow-up study at one hospital, Prof. Rosenhan asked staff to rate patients seeking admission on a 10-point scale, from “highly likely to be a (healthy) pseudo-patient” (1 or 2) to “least likely to be a pseudo-patient.” Staff were aware of the previous study and told one or more pseudo-patients would be sent their way unannounced. Forty-one (21.24%) of 193 patients received a 1 or 2 score. No pseudo-patients were, in fact, sent.
- These findings provided convincing evidence against the accuracy and validity of psychiatric diagnoses.
- The current state of psychiatric diagnoses is still broadly at odds with recent neurological findings, leading to uncertainty regarding their accuracy. Several interventions are proposed or underway to correct this. None counts with widespread support yet.

Aim
In the years leading to 1973, professor of law and psychology at Stanford University, Mr. David L. Rosenhan, sought to investigate whether psychiatrists actually managed to tease normal and abnormal psychological states apart. As Prof. Rosenhan put it:
At its heart, the question of whether the sane can be distinguished from the insane (and whether degrees of insanity can be distinguished from each other) is a simple matter: do the salient characteristics that lead to diagnoses reside in the patients themselves or in the environments and contexts in which observers find them?
The recent publication of the APA’s DSM II in 1968 underscored the popular belief among practitioners that psychiatric conditions could be distinguished from each other and from normal psychiatric good health, much like physiological diseases can be distinguished from each other and from good health itself.
In the 1960s, an increasing number of critiques of this belief emerged, arguing that psychiatric diagnoses were not as objective, valid, or substantive as their physiological counterparts, but were rather more like opinions and, therefore, subject to implicit biases even when propounded by competent psychiatrists or psychologists.
Prof. Rosenhan set out to settle the matter empirically. He resolved to have people with no current or past symptoms of serious psychiatric disorders admitted to psychiatric hospitals.
If their lack of abnormal psychiatric traits were always detected, he reasoned, we would have good evidence that psychiatrists were able to tell normal from abnormal psychiatric states. Psychiatric normality, it was presumed, was distinct enough from abnormality to be readily recognized by competent practitioners.
Sample
Nine participants, including Prof. Rosenhan, were recruited. All were deemed to have no present or past symptoms of serious psychiatric disorders. Each gained admission to one of nine distinct hospitals.
In eight cases, admittance was gained without the hospital’s staff’s foreknowledge.
In Prof. Rosenhan’s case, the hospital administrator and chief psychologist knew of their hospital’s inclusion in the study. Data from Prof. Rosehan’s stay or stays were not excluded.
Data from one participant were excluded due to a protocol breach (falsification of personal history beyond that of name, occupation, and employment). Between one and four of the remaining eight participants thereafter gained further admission to four other hospitals.
Data from 12 hospital stays, at 12 different hospitals, by eight participants were included in the study. Five of the included participants were male adults; three were female adults. Five worked or were engaged in psychology or psychiatry.
One of the 12 hospitals was privately funded; the rest received public funding. An undisclosed number of hospitals were “old and shabby” or “quite understaffed.”
The 12 hospitals were located in five states in the East and West coasts of the US.
Procedure
The admittance, stay, and discharge process was as follows —
- Participants set up an appointment at one of the hospitals under a false name, occupation, and employment.
- At the appointment, participants complained they had been hearing unfamiliar, often unclear voices which seemed to come from someone of their own sex and which seemed to say “empty,” “hollow,” and “thud;” participants provided truthful information on all matters other than name, occupation, and employment, with names, occupations and employment information of friends and family changed to fit with the participant’s assumed name, occupation, and employment.
- On admittance, participants stopped simulating any psychiatric symptoms, though there were a few cases of “brief[,] … mild nervousness and anxiety” which “abated rapidly.”
- In psychiatric wards, participants engaged with patients and staff as they would normally with colleagues in everyday life. When asked by staff how they were feeling, participants indicated that they were fine and that they no longer experienced symptoms. They received but did not ingest their prescribed medication, except in one or two instances. They recorded their observations regarding the ward, staff, and patients.
- Participants were discharged when the hospital’s staff responsible for their stay saw fit. A writ of habeas corpus was kept on file for each participant an undisclosed number of days after the study began.
- Between one and four participants repeated this process at four other hospitals.
Two further protocol breaches, which did not result in exclusion, were reported. One participant revealed their occupation in psychology to staff members. Another “attempted a romance with a nurse,” revealed their occupation in psychology to staff members, and provided psychotherapy to fellow patients.
Nursing reports for an undisclosed (“most”) number of the 12 stays were obtained from the hospitals. Coding protocols and training were not reported.
Depersonalization Observations
At four of the 12 hospitals, staff responses to patient-initiated contact were also investigated.
During their stay, four participants approached staff members with a request of the form, “Pardon me, Mr. [or Dr. or Mrs.] X, could you tell me when I will be eligible for grounds privileges?” or “… when I will be presented at the staff meeting?” or “… when I am likely to be discharged?”
No staff member was approached more than once a day. Staff responses were recorded.
Criteria for response classification, recording protocols, and pre-study training were not disclosed.
At six of the 12 hospitals, patients’ daily contact with staff (in minutes), from the initial admission interview to the final discharge meeting, inclusive of both, was measured.
Measurement protocol and pre-study training were not disclosed.
Non-existent Imposter Study
A second study was arranged at a research and teaching hospital in an undisclosed location. Its staff were aware of the first study’s results.
They were informed that one or more persons, previously instructed to simulate at least one symptom of a psychiatric disorder, i.e., a pseudo-patient, would attempt to gain admission within the following three months.
Staff were asked to rate each patient seeking admission on a ten-point scale, from most likely to be a pseudo-patient (1 or 2 on the scale) to least likely. No participants were, in fact, sent to the hospital. Scores were obtained for 193 patients.
No patients were independently evaluated by Prof. Rosenhan or affiliated researchers. No scoring protocol nor pre-study training was reported.
Findings
In eleven instances, participants were admitted on a diagnosis of schizophrenia and discharged with a diagnosis of schizophrenia in remission.
In one instance, a participant was admitted on a diagnosis of manic-depressive psychosis; their discharge diagnosis was not reported. Stays ranged from 7 to 52 days, with a mean of 19 days. Standard deviation was not disclosed.
Nursing reports “uniformly indicate[d] that the [participants] were “friendly,” “cooperative,” and “exhibited no abnormal indications.” Coding results and statistical significance were not reported.
Participants’ visitors “could detect no serious behavioral consequences [of hospitalization in participants].” No information on data collection from said visitors, nor statistical analyses on these data, were reported.
The errant diagnosis on admission, Prof. Rosenhan noted, could simply be attributed to physicians’ strong bias towards type II errors. As he put it:
The reasons [for this strong bias] are not hard to find: it is clearly [less] dangerous to misdiagnose illness than health. Better to err on the side of caution, to suspect illness even among the healthy.
Errant diagnoses after admission, once participants had dropped all pretense of psychiatric disturbance, were more surprising and troubling to Prof. Rosenhan.
It seemed that once diagnosed with an aberrant psychiatric trait, participants were unable to escape the diagnosis, despite their having dropped the farce immediately upon admission.
It was presumed that a competent practitioner, upon being well-acquainted with participants, would eventually identify the initial diagnosis as a type II error and subsequently correct it. No such correction took place in any of the 12 hospital stays.
The admission diagnoses seemed, in Prof. Rosenhan’s words, “so powerful that many of the [participants’] normal behaviors were overlooked entirely or profoundly misinterpreted.”
Prof. Rosenhan offered the following explanation for this surprising result. Persons not diagnosed with a mental illness, nonetheless, at times, exhibit “aberrant” behavior, like pacing around or frequently writing. Without a psychopathic diagnosis, these behaviors are attributed to something other than psychopathy, like being bored or being a writer.
But in the presence of such a diagnosis, these behaviors are more often attributed to psychopathy, as they were in two instances in the study than not. This attribution, in turn, only reinforces the diagnosis, thereby fixing any type II errors in place.
The fact that such behaviors are often attributed to psychopathies in diagnosed patients, Prof. Rosenhan argued, points more to the “enormous overlap in behaviors of the sane and the insane” than to the competence of psychiatrists, psychologists, or nurses.
Depersonalization Observations
On initiating contact with staff members, participants were overwhelmingly not paid any attention by psychiatrists, nurses, or attendants at four of the hospitals. Inter-hospital differences were not deemed significant and were not reported. Statistical differences and significance were not reported.
Six participants, totaling 129 days of hospitalization, measured their daily contact with staff. Daily contact with psychiatrists, psychologists, residents, and physicians ranged from 3.9 to 25.1 minutes, with a mean of 6.8 minutes. Disaggregated data, contact time with other staff, statistical differences, statistical significance, and standard deviation were not reported.
Contact, Prof. Rosenhan notes, indicates “concern and individuation,” its lack, “avoidance and depersonalization.” Staff’s overwhelming avoidance of patients, Prof.
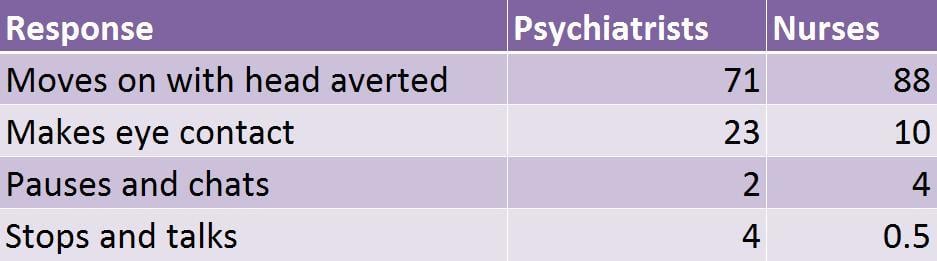
Table 1. Self-initiated contact by participants with psychiatrists, nurses, and attendants. Adapted from Table 1 of the 1973 Rosenhan study, p. 255. Copyright (c) 1973 AAAS.
Rosenhan notes resulted in an “overwhelming sense of powerlessness which invades the individual as he is continually exposed to the depersonalization of the psychiatric hospital.”
The import of this practice, and the powerlessness it elicited, Prof. Rosenhan argued, could be readily inferred.
[H]ow many patients might be “sane” outside the psychiatric hospital but seem insane in it_—not because craziness resides in them, as it were, but because they are responding to a bizarre setting … ?
Non-existent Imposter Study
Of the 193 scores obtained, 41 patients were judged highly likely to have been a pseudo-patient by at least one staff member, 23 by at least one psychiatrist, and 19 by one psychiatrist and at least one other staff member. No pseudo-patients were sent by Prof. Rosenhan or affiliated researchers.
Of the 41 patients judged highly likely to have been pseudo-patients —
- Either they did not, in fact, have any abnormal psychiatric symptoms and were correctly judged pseudo-patients by the staff;
- Or they did, in fact, have abnormal psychiatric symptoms (as presumed by the fact that they wished to be admitted), in which case the staff misdiagnosed them as pseudo-patients and thereby made a type I error in seeking to avoid type II errors.
In either case, Prof. Rosenhan pointed out the results indicated “that the tendency to designate sane people as insane can be reversed when the stakes (in this case, prestige and diagnostic acumen) are high.”
But it is notable that, in the second case, the price for avoiding type II errors might just be a higher type I error rate.
Conclusion
It is clear that we cannot distinguish the sane from the insane in psychiatric hospitals. The hospital itself imposes a special environment in which the meanings of behaviour can easily be misunderstood.
Both practitioners and patients, the study reveals, seem caught in Catch-22s. Out of an excess of caution, psychiatrists and psychologists strongly tend towards type II errors on admission. But once said error is made, there’s a slim chance it will be caught during in-patient treatment.
On the other hand, should practitioners try to avoid type II errors from sticking to patients, they run the risk of equally damaging type I errors. On the other hand, patients, once admitted, are likely to develop psychopathies, whether they truly had any on admission or not, given the bizarre setting they are thrust into on admittance.
But should they seek to avoid the setting — the psychiatric hospital — they run the risk of an untreated mental illness getting worse, in the case they truly suffered one, to begin with.
A way out for practitioners and patients is not immediately clear to Prof. Rosenhan. Two promising directions he noted were —
- The avoidance of psychiatric diagnoses of the form encouraged by the DSM II in favor of diagnosing patients with “specific problems and behaviors” so as to provide treatment outside of psychiatric hospitals and to keep any diagnostic label from “sticking” to a patient;
- Increasing “the sensitivity of mental health workers and researchers to the Catch-22 position of psychiatric patients,” for e.g., by having them read pertinent literature.
Other Conclusions
A good number of the study’s shortcomings should give us pause when drawing conclusions. Sampling, randomization, control, blinding, and statistical analysis methods were largely unreported and so likely not to have been up to present-day standards.
Participant training was not reported and so likely not undertaken before the study. No data on participants’ visitors and their evaluations were reported.
Study flaws aside, the observed effects were large enough to likely be clinically, and easily statistically, significant —
- All 12 hospitalizations resulted in type II errors both on admission and discharge;
- 2.94% of the 1,468 recorded participant-initiated interactions with psychiatric staff resulted in verbal engagement with the participant;
- 9.84% of the 193 patients scored at a research and teaching hospital were deemed very likely to have had no psychopathic traits on admission by both a psychiatrist and at least one other staff member.
The findings pointed to an unacceptable preponderance and persistence of type II errors by competent psychiatric staff and to the danger of psychiatric harm to patients posed by then-current psychiatric practices.
Critical Evaluation
Was the sample representative?
Field experiments have the major advantage of being conducted in a real environment and this gives the research high ecological validity. However, it is not possible to have as many controls in place as would be possible in a laboratory experiment.
Participant observation allows the collection of highly detailed data without the problem of demand characteristics. As the hospitals did not know of the existence of the pseudopatients, there is no possibility that the staff could have changed their behavior because they knew they were being observed.
However, this does raise serious ethical issues (see below) and there is also the possibility that the presence of the pseudopatient would change the environment in which they are observing.
Was the sample representative?
Strictly speaking, the sample is the twelve hospitals that were studied. Rosenhan ensured that this included a range of old and new institutions as well as those with different sources of funding.
The results revealed little differences between the hospitals. This suggests that it is probably reasonable to generalize from this sample and suggest that the same results would be found in other hospitals.
Prof. Rosenhan’s 1973 paper does not detail —
- How his sample size was determined, nor how his sample was selected;
- The study’s inclusion/exclusion criteria;
- How past or present serious psychiatric symptoms were diagnosed, nor by whom;
- Whether past or present mild to moderate psychiatric symptoms were diagnosed, nor by whom;
- How hospitals were selected;
- How participants were matched with false names, occupations, and employment information;
- How participants were matched with hospitals.
What type of data was collected in this study?
There is a huge variety of data reported in this study, ranging from quantitative data detailing how many days each pseudopatient spent in the hospital and how many times pseudopatients were ignored by staff to qualitative descriptions of the experiences of the pseudopatients.
One of the strengths of this study could be seen as the wealth of data that is reported and there is no doubt that the conclusions reached by Rosenhan are well illustrated by the qualitative data that he has included.
Was the study ethical?
Strictly speaking, no. The staff were deceived as they did not know that they were being observed and
you need to consider how they might have felt when they discovered the research had taken place.
Was the study justified? This is more difficult as there is certainly no other way that the study could have been conducted and you need to consider whether the results justified the deception. This is discussed later under the heading of usefulness.
What does the study tell us about individual/situational explanations of behavior?
The study suggests that once the patients were labeled, the label stuck. Everything they did or said was interpreted as typical of a schizophrenic (or manic-depressive) patient. This means that the situation that the pseudopatients were in had a powerful impact on the way that they were judged.
The hospital staff was not able to perceive the pseudopatients in isolation from their label and the fact that they were in a psychiatric hospital, and this raises serious doubts about the reliability and validity of the psychiatric diagnosis.
What does the study tell us about reinforcement and social control?
The implications of the study are that patients in psychiatric hospitals are ‘conditioned’ to behave in certain ways by the environments that they find themselves in.
Their behavior is shaped by the environment (nurses assume that signs of boredom are signs of anxiety, for example) and if the environment does not allow them to display ‘normal’ behavior, it will be difficult for them to be seen as normal.
Labeling is a powerful form of social control. Once a label has been applied to an individual, everything they do or say will be interpreted in the light of this label.
Rosenhan describes pseudopatients going to flush their medication down the toilet and finding pills already there. This would suggest that so long as the patients were not causing anyone any trouble, very few checks were made.
Was the study useful?
The study was certainly useful in highlighting the ways in which hospital staff interact with patients. There are many suggestions for improved hospital care/staff training that could be made after reading this study.
However, it is possible to question some of Rosenhan’s conclusions. If you went to the doctor falsely complaining of severe pains in the region of your appendix and the doctor admitted you to the hospital, you could hardly blame the doctor for making a faulty diagnosis.
Isn’t it better for psychiatrists to err on the side of caution and admit someone who is not really mentally ill than to send away someone who might be genuinely suffering?
This does not entirely excuse the length of time that some pseudopatients spent in the hospital acting perfectly normally, but it does go some way to supporting the actions of those making the initial diagnosis.
Outlook of Diagnostic Accuracy
Psychiatric diagnoses continue to be made as they were at the time of Prof. Rosenhan’s study — largely on the basis of inferences drawn from patient self-reports and practitioners’ observations of patient behavior and largely on the basis of criteria set by the APA’s DSM. This suggests two sources of diagnostic problems in psychiatry —
- the evidence used to reach a diagnosis, and
- the criteria by which said evidence is evaluated in reaching a diagnosis.
The evidence available to psychiatrists and psychologists in diagnosing mental disorders has long been much sparser than that available to other physicians.
There have been advances in the etiology of mental disorders — the relevant MeSH term now counts over 370,000 articles in PubMed, 4.00% of which are RCTs, meta-analyses, or systematic reviews. This growing corpus has yet to yield diagnostic tests, though.
In 2012, a group of three psychiatrists, led by Prof. Shitij Kapur of King’s College London, argued that a number of reasons were responsible for this lag, including widespread methodological shortcomings and the DSM’s classification itself.
On that note, the DSM has left much to desire. As Mr. Thomas Insel, former director of the NIMH, put it —
Unlike our definitions of ischemic heart disease, lymphoma, or AIDS, the DSM diagnoses are based on a consensus about clusters of clinical symptoms, not any objective laboratory measure.
Since its first publication in 1958, the DSM has reached a classification of mental disorders without data on their biological underpinnings.
Its nosology is increasingly at odds with aetiological research, which increasingly suggests that mental disorders are rather gradual deviations from typical brain functions.
This, in turn, suggests that mental disorders should be classified as points or areas on spectra rather than the neat categories propounded by the DSM. One effort at building such a nosology was begun by the NIMH in 2010.
The project dubbed the RDoC, is still confined to research, and is not ready for clinical application.
The myriad problems in psychiatric research and practice preclude any consensus on the accuracy of psychiatric diagnoses and are likely to do so until they are resolved.
The field has not converged on a corrective program, though there exist a number of such programs competing for widespread support.
FAQs
What did the Rosenhan study suggest in 1973?
The Rosenhan study in 1973 suggested that psychiatric diagnoses are often subjective and unreliable. Rosenhan and his associates feigned hallucinations to get admitted to mental hospitals but acted normally afterward.
Despite this, they were held for significant periods and treated as if they were genuinely mentally ill. The study highlighted issues with the validity of psychiatric diagnosis and the stigma attached to mental illness.
What did the classic study by Rosenhan reveal about the power of labels that are applied to individuals?
The classic study by Rosenhan showed the influential effect of labels on individuals, specifically psychiatric labels. By pretending to have hallucinations, mentally healthy participants gained admission to psychiatric hospitals.
The study demonstrated that once labeled as mentally ill, their behaviors were consistently interpreted in that context, even when they stopped simulating symptoms.
References
Adam, D. (2013). On the spectrum. Nature, 496(7446), 416.
Insel, T. .R. (2013, 29th April). Transforming Diagnosis. [Weblog]. Retrieved 4 November 2020, from https://www.nimh.nih.gov/about/directors/thomas-insel/blog/2013/transforming-diagnosis.shtml
Kapur, S., Phillips, A. G., & Insel, T. R. (2012). Why has it taken so long for biological psychiatry to develop clinical tests and what to do about it?. Molecular psychiatry, 17 (12), 1174-1179.
Rosenhan, D. L. (1973). On being sane in insane places. Science, 179( 4070), 250-258.
Sharp, C., Fowler, J. C., Salas, R., Nielsen, D., Allen, J., Oldham, J., Kosten, T., Mathew, S., Madan, A., Frueh, B. C., & Fonagy, P. (2016). Operationalizing NIMH Research Domain Criteria (RDoC) in naturalistic clinical settings. Bulletin of the Menninger Clinic, 80 (3), 187–212.

