On This Page:
Occipital Lobe Location
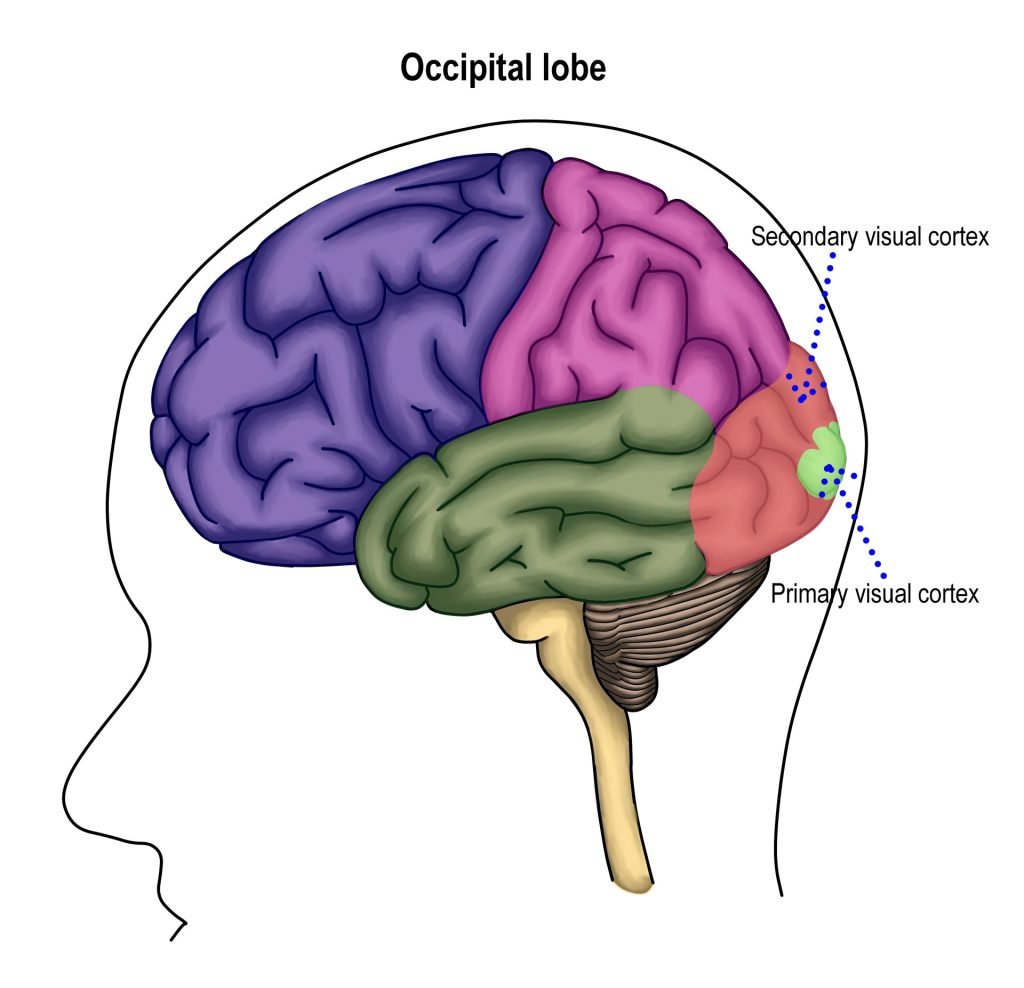
The occipital lobe is located at the very back of the brain and contains the primary visual cortex, which is responsible for interpreting incoming visual information.
It is the smallest lobe of the brain, accounting for around 12% of the total surface area of the brain’s cortex. It is located at the rear of the brain, behind the temporal and parietal lobes, and below the occipital bone of the skull.
There are two sides to the occipital lobes, in both the left and right hemispheres of the brain, separated by a cerebral fissure (a deep groove separating the two cerebral hemispheres).
The occipital lobe essentially receives sensory information from the retinas of the eyes, of which, is then encoded into different visual data, such as color, orientation, and motion.
Occipital Lobe Functions
Below is a list of some of the associated functions of the occipital lobes:
- Assessing size, depth, and distance
Determining color information- Object recognition
- Face recognition
- Mapping the visual world
- Movement
Researchers once believed that the occipital lobe’s only function was to control visual functions. However, we now understand the occipital lobe to be involved in other functions due to being able to receive input from other brain regions.
The occipital lobes transmit visual information to the temporal lobes, which aids in giving meaning to visual information, storing memories, and responding to external stimuli in the world.
An interesting phenomenon relating to the occipital lobes is called synaesthesia. This is a perceptual experience some people have whereby specific events in one sensory modality induce experiences in another.
For instance, a type of synaesthesia called color-graphemic synaesthesia relates to people perceiving colored experiences with numbers or written letters. Therefore, they may attribute the letter ‘A’ with the color red, or the number ‘4’ with the color yellow.
Substructures
The occipital lobes can be divided into several functional areas, although no anatomical markers distinguish these areas.
Brain imaging has revealed that neurons in the occipital cortex create an ongoing visual map of information taken in by the retinas.
Similarly, it is worth noting that the motor cortex plays a role in the muscles of the eyes, which are heavily relied on by the occipital lobes.
Primary Visual Cortex
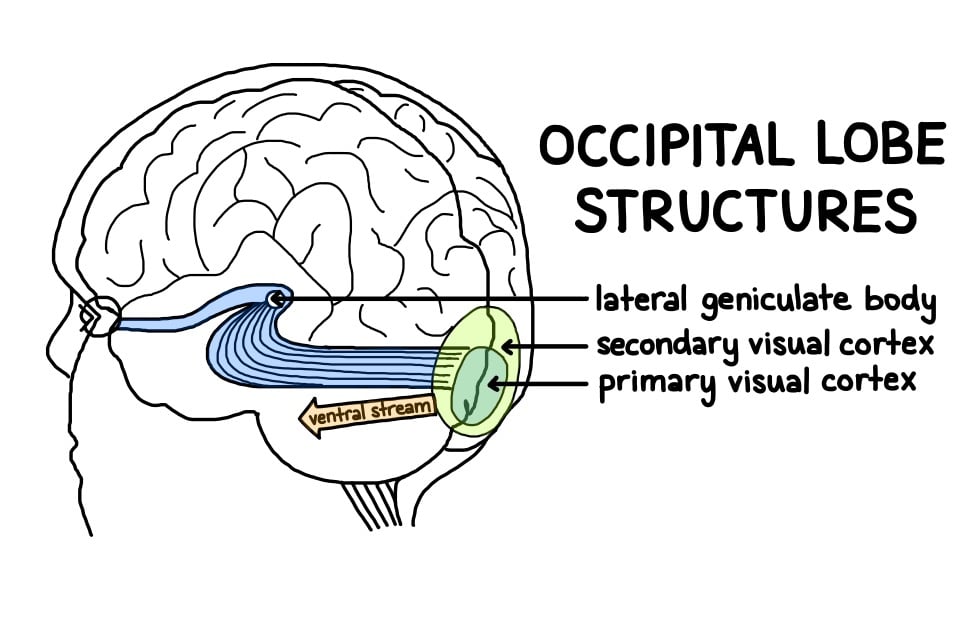
This section is also known as Brodmann area 17, or visual area V1. The primary visual cortex receives sensory information from the eyes’ retinas, then transmits information relating to location, spatial data, motion, and the colors of objects in the field of vision.
This information gets transported via two streams: the dorsal and ventral streams. The visual cortex is divided into six areas depending on the function and structure of each area, referred to as V1, V2, V3, V4, and V5.
Secondary Visual Cortex
This section is also known as Brodmann area 18 and 19, or visual area V2. This is the area immediately surrounding the primary visual cortex.
It receives information from the primary visual cortex for further organization of visual input. It also passes information to visual areas V3, V4, and V5.
Ventral Stream
The secondary visual cortex also encompasses the ventral stream, which allows information to flow to temporal lobe structures to enable us to process what objects are.
Without the ventral stream, we would still be able to see normally, but without conscious awareness or understanding of what we are seeing.
Lateral Geniculate Bodies
The lateral geniculate body is part of the thalamus and acts as a sensory relay system. Raw information coming from the outer part of the retinas enters this area for processing before being sent to the primary visual cortex.
Lingula
The lingula is also responsible for processing vision by gathering information about what is in the field of vision from the side half of the retina. Together with the help of the lateral geniculate bodies, the lingula creates spatial awareness and gives depth to visual information.
Dorsal Stream
The dorsal stream allows information to flow from the occipital lobes to the parietal lobes in order for us to process where objects are located. The dorsal stream connects to both the V1 and V2 regions, allowing these areas to send information about the size and shape of objects in our field of vision.
Damage
Below is a list of symptoms that may occur if an individual has experienced damage within their occipital lobe:
- Blindness
- Hallucinations
- Difficulty locating objects
- Changes in depth perception
- Difficulties identifying colors
- Difficulties in reading and writing
- Inability to see color, orientation, and motion
Synaesthesia - Difficulty recognizing drawn objects
The occipital lobes at the back of the brain make it less susceptible to damage. As with many brain regions, if a part of the occipital lobe becomes damaged, other brain areas can compensate for this damage, meaning overall function is not fully affected. Complete damage to the primary visual cortex, however, can cause cortical blindness.
As the visual field is essentially mapped onto the surface of the primary visual cortex, a small bit of damage can cause a ‘hole’ in a specific part of the field of vision.
Damage to the primary visual cortex could also affect the way a person recognizes objects by sight. For instance, when presented with a mobile phone and asked to identify it, they may say they can see a screen and some buttons but may not be able to name the actual object as a whole. However, if given the phone to hold, they would be able to recognize what it is through touch.
Similarly, they may not be able to recognize who is standing in front of them by sight. Once they hear the voice of the person, they would then be able to recognize them by sound. This deficit is known as visual agnosia.
Another interesting but exceedingly rare condition is called Riddoch Syndrome. This is a condition whereby an individual is unable to view stationary objects in their field of vision. They can only, however, view people or objects if they are moving.
Surgery has proven successful in patients who have occipital lobe epilepsy.
However, it is difficult to identify the entire area of the issue through brain imaging and this has sometimes led to post-operative visual deficit after surgery (Harward et al., 2018).
A way to strengthen the occipital lobes is to exercise it with visual activities.
This could include visualization exercises, watching a 3D movie or driving without GPS navigation. Completing exercises like these should aid in enhancing visual-spatial skills.
Research Studies
- Sperling et al. (2006) investigated the neural basis of color-grapheme synaesthesia using functional magnetic resonance imaging (fMRI). These findings showed that the grapheme-induced color perception in synaesthesia is caused by activation of the color areas of the visual cortex (V4).
- Kandel, Schwartz, & Jessell (1991) investigated damage within parietal-temporal-occipital association regions. They found that damage in this area can lead to word blindness with writing impairments, also known as alexia and agraphia.
- Park, Yoon, & Rhee (2011) completed neuropsychological tests on patients who had suffered damage to the occipital lobes after a stroke. This was used to test whether there were any executive function deficits in these patients. They found that memory impairments were the only area in which patients with isolated occipital lobe damage demonstrated a decline in performance. Only with additional damage to the temporal regions was executive dysfunction witnessed across numerous domains.
- Ishizaki et al. (2008) used positron emission tomography (PET) scans in individuals with depression. They found that differences in cerebral blood flow in the occipital lobe were correlated with depression. After the use of pharmacotherapy, they found that cerebral blood flow increased in the parieto-occipital regions.
- People with Autism typically show enhanced perceptual skills when engaged in visual search, visual discrimination, and embedded figure detection tasks. When completed these types of visual tasks, there has been shown to be more brain activity in the occipital lobes of these individuals when compared to neurotypical individuals (Samson, Mottron, Soulieres, & Zeffiro, 2011). Tate et al. (2007) used magnetic resonance imaging (MRI) on individuals with Autism and found significant overgrowth in the occipital cortex. Another study also found occipital lobe enlargement in those with Autism compared to a control group (Piven, Arndt, Bailey, & Andreasen, 1996).
- Binder et al. (2008) found that patients who had epilepsy of the occipital lobes had deficits in their visual function. Gülgönen et al. (2005) investigated the neurobiological functions of those with occipital lobe epilepsy. They found that these individuals performed lower on tests of attention, memory, and intellectual functioning, in comparison to a control group.
- As damage to the occipital lobe can cause visual hallucinations, this region has been investigated as a neurobiological correlate of those with schizophrenia (McCarley et al., 1999). Onitsuka et al. (2007) used MRI to investigate the brains of those with schizophrenia. They found that those with chronic schizophrenia had reduced grey matter (outermost area, containing neurons) volume in the visual association cortex, suggesting that this area is a cause of some of the visual deficits observed in those with schizophrenia.
References
Binder, D. K., Von Lehe, M., Kral, T., Bien, C. G., Urbach, H., Schramm, J., & Clusmann, H. (2008). Surgical treatment of occipital lobe epilepsy. Journal of Neurosurgery, 109 (1), 57-69.
Gülgönen, S., Demirbilek, V., Korkmaz, B., Dervent, A., & Townes, B. D. (2000). Neuropsychological functions in idiopathic occipital lobe epilepsy. Epilepsia, 41 (4), 405-411.
Harward, S. C., Chen, W. C., Rolston, J. D., Haglund, M. M., & Englot, D. J. (2018). Seizure outcomes in occipital lobe and posterior quadrant epilepsy surgery: a systematic review and meta-analysis. Neurosurgery, 82 (3), 350-358.
Ishizaki, J., Yamamoto, H., Takahashi, T., Takeda, M., Yano, M., & Mimura, M. (2008). Changes in regional cerebral blood flow following antidepressant treatment in late‐life depression. International Journal of Geriatric Psychiatry, 23 (8), 805-811.
Jessell, T. M. (1991). Principles of neural science (pp. 173-193). J. H. Schwartz, & E. R. Kandel (Eds.). New York: Elsevier.
McCarley, R. W., Wible, C. G., Frumin, M., Hirayasu, Y., Levitt, J. J., Fischer, I. A., & Shenton, M. E. (1999). MRI anatomy of schizophrenia. Biological Psychiatry, 45 (9), 1099-1119.
Onitsuka, T., McCarley, R. W., Kuroki, N., Dickey, C. C., Kubicki, M., Demeo, S. S., Frumin, M., Kikinis, R., Jolesz, F. A. & Shenton, M. E. (2007). Occipital lobe gray matter volume in male patients with chronic schizophrenia: A quantitative MRI study. Schizophrenia Research, 92 (1-3), 197-206.
Park, K. C., Yoon, S. S., & Rhee, H. Y. (2011). Executive dysfunction associated with stroke in the posterior cerebral artery territory. Journal of Clinical Neuroscience, 18 (2), 203-208.
Piven, J., Arndt, S., Bailey, J., & Andreasen, N. (1996). Regional brain enlargement in autism: a magnetic resonance imaging study. Journal of the American Academy of Child & Adolescent Psychiatry, 35 (4), 530-536.
Samson, F., Mottron, L., Soulières, I., & Zeffiro, T. A. (2012). Enhanced visual functioning in autism: An ALE meta‐analysis. Human Brain Mapping, 33 (7), 1553-1581.
Sperling, J. M., Prvulovic, D., Linden, D. E., Singer, W., & Stirn, A. (2006). Neuronal correlates of colour-graphemic synaesthesia: AfMRI study. Cortex, 42 (2), 295-303.
Tate, D. F., Bigler, E. D., McMahon, W., & Lainhart, J. (2007). The relative contributions of brain, cerebrospinal fluid-filled structures and non-neural tissue volumes to occipital-frontal head circumference in subjects with autism. Neuropediatrics, 38(01), 18-24.


