On This Page:
Dopamine is a neurotransmitter that serves as a chemical messenger in the brain. It can function as both an excitatory and inhibitory neurotransmitter, leading to diverse effects on the brain, body, and behavior.
Dopamine is primarily known to be associated with feelings of pleasure and rewards. This chemical can also contribute to feelings of:
-
Alertness
-
Focus
-
Motivation
-
Happiness
Dopamine is released when the brain is expecting a reward. The flood of dopamine to the brain when experiencing a pleasurable stimulus (e.g., delicious food, video games, sex) can reinforce wanting to engage with this stimulus more due to the pleasurable feeling it causes.
This is a cycle of motivation, reward, and reinforcement. When associating a certain activity with pleasure, sometimes even mere anticipation may be enough to raise dopamine levels.
The right amount of dopamine is ideal for learning, planning, and productivity. For instance, if someone has been working hard on a project for a long time, they can experience a surge of dopamine activity when it is finally completed.
Function of Dopamine
Dopamine is a neurotransmitter in the brain associated with pleasure, reward, motivation, and motor control. In psychology, it’s linked to feelings of gratification and is implicated in mood disorders, addiction, and certain behaviors when its levels are imbalanced.
Whilst strongly involved in pleasure and rewards, dopamine is also involved in other functions:
-
Motor functions
-
Mood regulation
-
Executive functioning
-
Memory and focus
-
Sleep
-
Digestion and blood flow
It is important to note that dopamine does not act in isolation. It works with other neurotransmitters and hormones, such as serotonin and adrenaline, to perform a variety of functions.
Dopamine is a chemical of the catecholamine and phenethylamine families. It was believed to be first identified by Kathleen Montagu in her 1957 paper demonstrating findings on key neurotransmitters.
As part of her research, she examined the quantities of norepinephrine, epinephrine, and 3-hydroxytryramine from extracted tissues of the brains of several species.
Montagu speculated that there might be an additional catecholamine similar to hydroxytyramine, which she later confirmed to be what is known as dopamine.
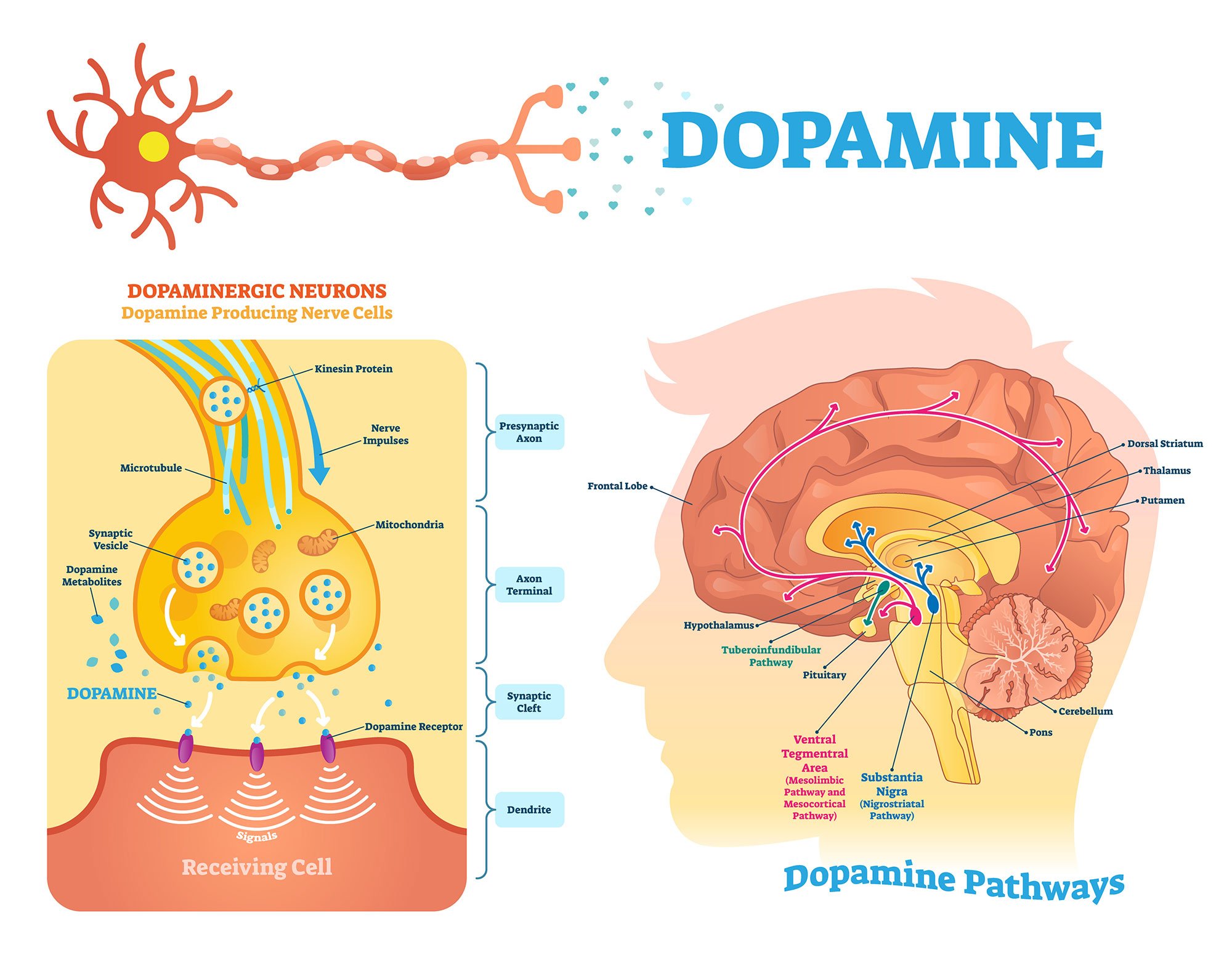
Dopamine is highly concentrated in areas of the brain called the substantia nigra and the ventral tegmental area (VTA) in the midbrain. Other brain areas dopamine can be made are the hypothalamus and the olfactory bulb.
There are dopamine pathways that can be triggered when exposed to a stimulus that is rewarding, resulting in increased amounts of dopamine circulating around brain areas.
Role Of Dopamine On Learning And Motivation
Reward System
Dopamine plays a key role in the brain’s reward system. This neurotransmitter helps to reinforce certain behaviors that result in a reward.
In classical studies of rats, a surge of dopamine prompts the animal to press a lever to get a pellet of food repeatedly.
This works the same way in humans, for instance, choosing to eat more pleasurable food, such as another slice of cake, because we have enjoyed the rewarding feeling the food has given us.
Reward Prediction
Some lines of study have found that midbrain dopamine neurons can be activated by proximal contact (touch, taste) with unexpected rewards.
When such events became predictable, the neurons were found to respond to the more distal (visual or auditory) stimuli that precede and predict the availability of the reward.
The neurons would then stop responding to the proximal contact with the reward (Romo & Schultz, 1990; Schultz et al., 1992).
This may be an oversimplification as the neurons that are no longer reactive to the proximal reward stimuli have been found to still be responsive to the lack of the reward.
When the expected proximal contact does not occur, the dopamine neurons become inhibited. So, although dopamine release is triggered by the earliest reliable predictor of reward, midbrain dopamine remains sensitive to the receipt or lack of reward.
The anticipation of expecting a reward was studied by researchers in a game of chance.
In the anticipation phase, where participants were told they might win money, blood flow was found in the amygdala and frontal cortex, indicating activity in the nucleus accumbens and the hypothalamus, all rich in dopamine receptors.
The bigger the potential reward, the greater dopamine-led brain activity was found.
Conditioned reinforcement
By allowing dopamine to affect choices, it can bias towards choosing the stimulus that was learned from the amount of positive or negative reinforcement the stimulus received.
Reward-associated motivational stimuli can serve as conditioned reinforcers when given after a response.
For instance, in a study on rats, when they were thirsty, they learned to work for the presentation of a light that was previously paired with water.
In this test, injections of amphetamine into the nucleus accumbens (a reward area of the brain) caused dopamine release. They enhanced response to the light (Taylor & Robbins, 1984), whereas dopamine-selective lesions of the nucleus accumbens reduced this response (Taylor & Robbins, 1986).
Therefore, dopamine can modulate the expression of conditioned reinforcement as well as is essential for the establishment of conditioned reinforcers.
What Dopamine Does In The Brain
Within the brain are dopamine receptors which are proteins found in the brain, neurons, and the body. As a dopamine signal approaches a nearby neuron, it attaches to that neuron’s receptor.
The receptor and neurotransmitter work like a lock and key. The dopamine attaches to the dopamine receptor, delivering its chemical message by causing changes to occur in the neuron which received the signal.
Through the use of dopamine receptors, the effects of dopamine, such as movement coordination, pleasure, and cognition, can take effect.
Where is dopamine produced?
Dopamine is mostly produced in an area of the brain called the ventral tegmental area (VTA); a dopamine-rich nucleus located within the midbrain.
Once produced in the VTA, dopamine is transported to other areas of the brain through different dopamine pathways, the two main ones being the mesolimbic and the mesocorticol pathways. Other pathways include the nigrostriatal and tuberoinfundibular pathways.
Dopamine pathways are neuronal connections in which dopamine travels to areas of the brain and body to convey important information such as executive thinking, cognition, feelings of reward and pleasure, and voluntary movement.
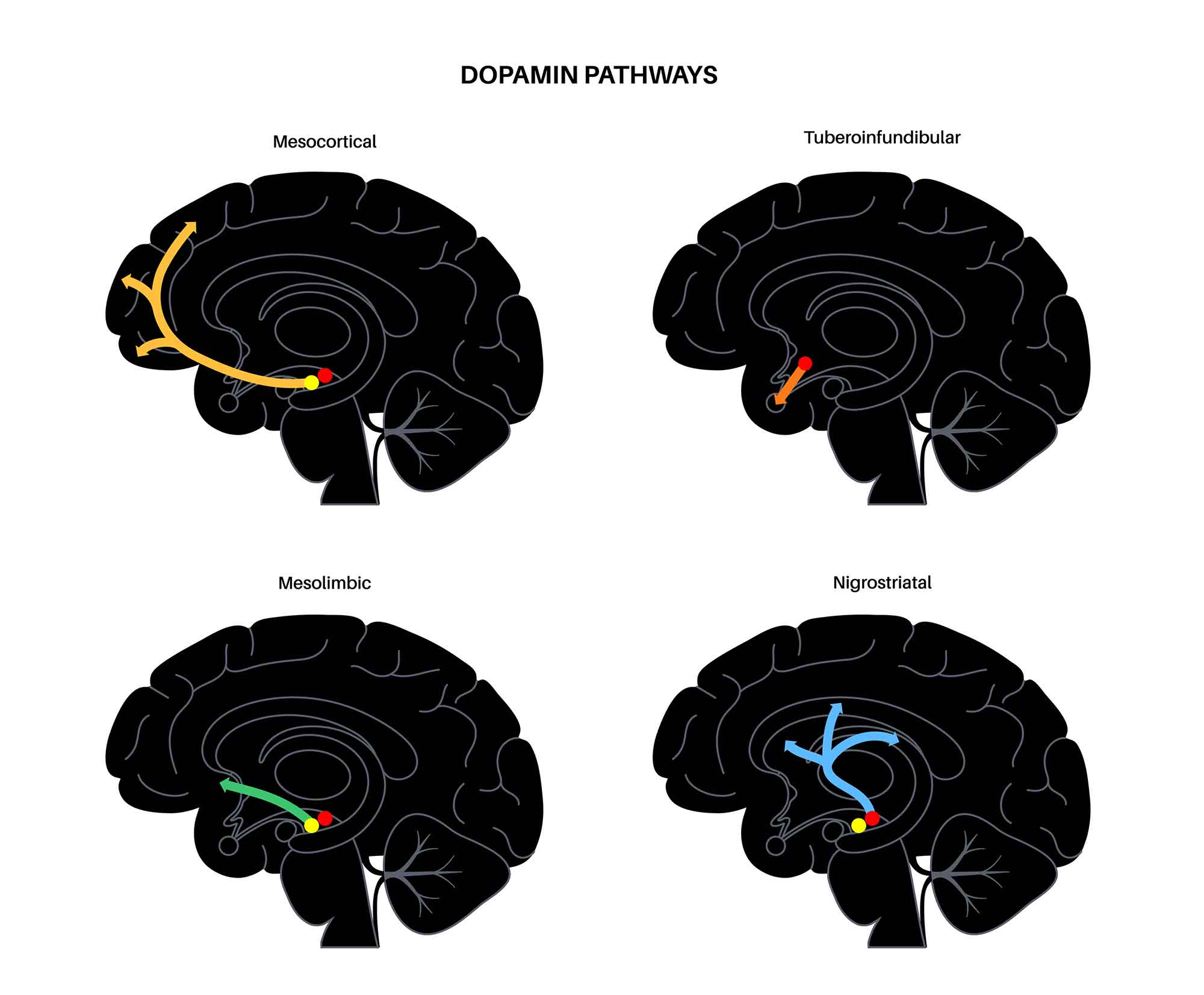
Mesolimbic pathways
This dopamine pathway is highly involved in the functions of pleasure and reward. Beginning at the VTA, dopamine produced here projects to the nucleus accumbens.
When here, dopamine primarily mediates feelings of pleasure and reward. For instance, if someone eats a food they enjoy, dopamine is released from the VTA to the nucleus accumbens which then creates positive feelings that reinforce the behavior.
Sometimes stimuli can create intense feelings of euphoria.
The nucleus accumbens is found in the ventral striatum and is part of a complex circuit involving the amygdala and the hippocampus. The activation of the mesolimbic dopamine pathway communicates that it wants to repeat what just happened in order to feel the rewarding sensation again.
Since the nucleus accumbens has connections to the amygdala, a region of the limbic system associated with emotions, this attributes feelings towards the experienced reward.
Likewise, connections to the hippocampus, an area associated with memory, can attribute memories of pleasure to the experience to reinforce this sensation to happen again.
Stimulating the nucleus accumbens is important for daily activities, but over-stimulation can result in cravings for the stimulus which stimulates it.
Mesocorticol pathways
As with the mesolimbic pathways, the mesocortical pathway starts with dopamine projections originating from the VTA. From the VTA, signals are sent to the prefrontal cortex, an area involved in cognition, working memory, and decision-making.
Thus, activation of this pathway brings about the conscious experience of the pleasure and reward being experienced. Attention, concentration, and decisions can be made as a result of pleasure and reward.
Dysfunction in this pathway can therefore result in poor concentration and an inability to make decisions.
Nigrostriatal pathways
This dopamine pathway is involved in motor planning. The dopamine projections start in the substantia nigra, a basal ganglia structure located in the midbrain.
These projections go to the caudate and putamen, which are also parts of the basal ganglia. The neurons in this pathway stimulate purposeful movement and contain about 80% of the dopamine in the brain.
If there are reductions in the number of dopamine neurons in this pathway, this can result in motor control impairments, including movement disorders such as Parkinson’s disease.
Symptoms of dysfunction in this pathway may include spasms, contractions, tremors, and motor restlessness.
Tuberoinfundibular pathways
The dopamine neurons in this pathway originate in the hypothalamus, an area that plays a role in hormone production and helps to stimulate many important processes in the body.
Specifically, the neurons are in the arcuate and periventricular nuclei of the hypothalamus. These then project to the infundibular region of the hypothalamus. In this pathway, dopamine is released into the portal circulation that connects this region to the pituitary gland.
Here, dopamine functions to inhibit prolactin release. Prolactin is a protein secreted by the pituitary gland that enables milk production and has important functions in metabolism, sexual satisfaction, and the immune system.
Dopamine Hypothesis In Schizophrenia
The dopamine hypothesis for schizophrenia suggests that some of the symptoms of schizophrenia involve excess dopamine activity.
The dopamine hypothesis of schizophrenia was derived from observations in the 1960s where the effects of amphetamines resembled schizophrenia. Amphetamines increase dopamine function (Seeman et al., 1976).
Dopamine appears to play a big role in the activity of the frontal and temporal lobes, particularly parts of the cerebral cortex of these lobes that play a role in the cognitive, emotional, and perceptual functions that are often abnormal in schizophrenia.
However, inconsistencies in post-mortem findings and debates on whether certain changes were due to drugs or the disease made it challenging to pinpoint schizophrenia’s exact link with dopamine. Yet, imaging studies revealed that schizophrenic patients release more dopamine than healthy individuals (Laruelle et al., 1996).
The discovery of organic changes in the brains of schizophrenic patients through imaging techniques shifted the focus to viewing schizophrenia as a neurodevelopmental disorder.
This suggested that schizophrenia might stem from reduced dopamine function in the prefrontal cortex, leading to increased dopamine in other areas (mesolimbic). Potential treatments now consider balancing these levels, exemplified by drugs like aripiprazole (Carlsson, 1988).
There appear to be abnormalities in the mesocortical and mesolimbic pathways that carry dopamine from the VTA to areas of the cerebral cortex.
Disruptions in the parts of the cerebral cortex are believed to cause many of the cognitive symptoms of schizophrenia, such as disorganized thinking, difficulty integrating thoughts, and poor concentration.
Abnormal activity of dopamine pathways in the limbic system is believed to be responsible for many of the negative symptoms of schizophrenia, such as lack of motivation and social withdrawal.
Also, dopamine abnormalities in the temporal and prefrontal areas of the brain are believed to be overactive in those with schizophrenia and thus can lead to some of the positive symptoms of the condition, such as hallucinations and delusions.
This hypothesis appears to make sense since antipsychotic drug medication, which work to block dopamine receptor in the brain appear to be effective in treating the positive symptoms of schizophrenia.
Likewise, the effects of dopamine-enhancing drugs such as methamphetamine and cocaine, over repeated exposure, can gradually induce paranoid psychosis in non-schizophrenic people.
This well-documented observation shows that sustained increases in dopamine activity can cause some of the similar symptoms of schizophrenia.
However, the dopamine hypothesis for schizophrenia may be an oversimplification as there may be many more neuronal network abnormalities and neurotransmitter systems involved in causing the condition.
Research since the dopamine hypothesis has indicated that glutamate, GABA, acetylcholine, and serotonin alterations are also involved in the pathology of schizophrenia, so it may not be dopamine alone which affects this condition.
What about the future?
We know a lot about two types of dopamine receptors in the brain, but less about three others. Using special mice in research, scientists discovered the importance of the D5 receptor in male and female sexual behaviors. Also, some research shows mice might like sugar even if they can’t produce dopamine.
Notably, there’s a growing consensus that studying dopamine should not be in isolation but in conjunction with other transmitter systems. This integrated approach recognizes the broader neuronal organization and connectivity in the brain.
Even though dopamine neurons comprise less than 1% of brain neurons, alterations in dopamine levels or functions can significantly influence behavior.
This underscores the idea that dopamine’s primary role might be integrating information pertinent to biologically significant stimuli rather than transmitting specific data.
FAQs
What happens if dopamine is depleted?
Low dopamine levels may result in some of the following symptoms:
– Reduced alertness
– Difficulty concentrating
– A lack of motivation
– Poor coordination
– Movement difficulties
– Inability to feel pleasure
In more extreme cases, a lack of dopamine could result in conditions such as Parkinson’s disease, dopamine transporter deficiency syndrome, or depression.
Although dopamine alone may not directly cause depression, low levels of dopamine have been suggested to cause specific symptoms associated with this condition, such as motivational issues, feeling hopeless and helpful, and a loss of interest in previously enjoyed activities.
It’s suggested that these symptoms may be linked to a dysfunction in the dopamine systems of the brain. A main trigger for these dysfunctions could be due to stress, pain, lack of sleep, or trauma.
A physiological explanation is that there may be a diminished dopamine release from the presynaptic neurons and/or impairment in signal transduction, possibly due to changes in the number of dopamine receptors.
Attention deficit hyperactivity disorder (ADHD) is a condition that is also associated with low levels of dopamine.
Symptoms of ADHD include difficulties with concentration and attention, impulsiveness and finding it difficult to remain still.
Since people with ADHD have lowered dopamine levels, they are more likely to carry out behaviors in order to obtain more dopamine.
What are the symptoms of high dopamine?
High levels of dopamine can make people feel euphoric in the short term; however, over time, it can be detrimental. In excess, dopamine can be a contributing factor in mania, hallucinations, and delusions.
A surplus of dopamine can result in more competitive behaviors, aggression, poor control over impulses, gambling behaviors, and addiction.
As such, addictive drugs can increase levels of dopamine, encouraging the individual to continue to use these drugs to reach that pleasurable feeling of reward.
This does not just have to be an addiction to drugs; people can be addicted to anything which gives them a surge of dopamine, such as video games, food, and social media use.
How do I get my dopamine levels back to normal?
Depending on whether dopamine levels are too high or low will determine what techniques to take. If wanting to increase dopamine levels, some ways can include:
– Enduring a good sleep schedule
– Less screen time (e.g., television, phone), especially before bed
– Learning to meditate or undertaking mindfulness training
– Exercising regularly
– Changes in diet to increase levels of vitamin D and essential fatty acids
– Physical therapy for muscle stiffness and movement problems
Dopamine agonists – a class of drugs that bind to and activate dopamine receptors in the brain, mimicking the action of naturally-occurring dopamine in the brain.
For those with too much dopamine, such as individuals with schizophrenia, dopamine antagonists are usually recommended.
These are a class of drugs that bind to and block dopamine receptors, turning down the dopamine activity.
Many antipsychotic drugs are dopamine antagonists, including Chlorpromazine (Thorazine), Risperidone (Risperdal), and Clozapine (Clozaril).
What happens when you ‘dopamine fast’?
Dopamine fasting is a recent trend where people strive to ‘reset’ their dopamine levels by completely abstaining from anything that brings them pleasure. This can include phone use, social media, video games, delicious food, sex, and social interaction.
Taking breaks from behaviors that trigger strong amounts of dopamine release could allow the brain to recover and restore itself, being an antidote to the age of overstimulation we live in.
Kent Berridge, a professor of psychology and neuroscience, suggests that taking a break from a stimulating activity (or all of them) will not reset dopamine levels, but it can stop the dopamine system from turning on constantly.
Dopamine fast is not believed to be something that can reduce dopamine, but having breaks from one or two pleasurable activities at a time can help in reducing impulsive behaviors.
In addition, a specific study showed that dopamine fasting from the social media platform Facebook for a week helped students regain 13.3 hours of their time and significantly reduced depressive symptoms by 17%, which allowed them to engage in more healthy behaviors instead (Mosquere et al., 2019).
References
Brisch, R., Saniotis, A., Wolf, R., Bielau, H., Bernstein, H. G., Steiner, J., Bogerts, B., Braun, K., Jankowski, Z., Kumaratilake, J., Henneberg, M. & Gos, T. (2014). The role of dopamine in schizophrenia from a neurobiological and evolutionary perspective: old fashioned, but still in vogue. Frontiers in psychiatry, 5, 47.
Bridges, N. (2016, November 25). Dopamine Pathways. Sanesco. https://sanescohealth.com/blog/dopamine-pathways/
Cannon, C. M., Scannell, C. A., & Palmiter, R. D. (2005). Mice lacking dopamine D1 receptors express normal lithium chloride‐induced conditioned taste aversion for salt but not sucrose. European Journal of Neuroscience, 21(9), 2600-2604.
Carlsson, A. (1988). The current status of the dopamine hypothesis of schizophrenia. Neuropsychopharmacology: official publication of the American College of Neuropsychopharmacology, 1(3), 179-186.
Conrad, B. (n.d.). The Role of Dopamine as a Neurotransmitter in the Human Brain. Enzo. Retrieved 2021, November 5, from: https://www.enzolifesciences.com/science-center/technotes/2018/november/the-role-of-dopamine-as-a-neurotransmitter-in-the-human-brain/
Laruelle, M., Abi-Dargham, A., Van Dyck, C. H., Gil, R., D’Souza, C. D., Erdos, J., … & Innis, R. (1996). Single photon emission computerized tomography imaging of amphetamine-induced dopamine release in drug-free schizophrenic subjects. Proceedings of the National Academy of Sciences, 93(17), 9235-9240.
Mosquera, R., Odunowo, M., McNamara, T., Guo, X., & Petrie, R. (2020). The economic effects of Facebook. Experimental Economics, 23(2), 575-602.
Pietrangelo, A. (2019, November 5). How Does Dopamine Affect the Body? Healthline. https://www.healthline.com/health/dopamine-effects
Romo, R., & Schultz, W. (1990). Dopamine neurons of the monkey midbrain: contingencies of responses to active touch during self-initiated arm movements. Journal of neurophysiology, 63(3), 592-606.
Schultz, W., Apicella, P., Scarnati, E., & Ljungberg, T. (1992). Neuronal activity in monkey ventral striatum related to the expectation of reward. Journal of Neuroscience, 12(12), 4595-4610.
Seeman, P., Lee, T., Chau-Wong, M., & Wong, K. (1976). Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature, 261(5562), 717-719.
Sepah, C. (2019, August 7). The Definitive Guide to Dopamine Fasting 2.0 – The Hot Silicon Valley Trend. LinkedIn. https://www.linkedin.com/pulse/dopamine-fasting-new-silicon-valley-trend-dr-cameron-sepah/
Taylor, J. R., & Robbins, T. W. (1984). Enhanced behavioural control by conditioned reinforcers following microinjections of d-amphetamine into the nucleus accumbens. Psychopharmacology, 84(3), 405-412.
Taylor, J. R., & Robbins, T. W. (1986). 6-Hydroxydopamine lesions of the nucleus accumbens, but not of the caudate nucleus, attenuate enhanced responding with reward-related stimuli produced by intra-accumbens d-amphetamine. Psychopharmacology, 90(3), 390-397.
Wise, R. A. (2004). Dopamine, learning and motivation. Nature reviews neuroscience, 5(6), 483-494.

